- 1Postgraduate School of Clinical Pharmacology, Department of Oncology and Hemato-Oncology, University of Milan, Milan, Italy
- 2Department of Clinical Internal, Anesthesiological and Cardiovascular Sciences, Sapienza University of Rome, Rome, Italy
- 3Department of Oncology and Hemato-Oncology, University of Milan, Milan, Italy
- 4Central Pharmacy, ASST Spedali Civili, Brescia, Italy
- 5Experimental and Clinical Pharmacology Unit, Centro di Riferimento Oncologico di Aviano (CRO), IRCCS, Aviano, Italy
- 6Pharmacy Unit, ASST Papa Giovanni XXIII, Bergamo, Italy
- 7Oncology Department, Mario Negri Institute for Pharmacological Research IRCCS, Milano, Italy
- 8Department of Economics and Finance, University of Rome “Tor Vergata”, Rome, Italy
- 9Department of Laboratory Medicine, ASST Grande Ospedale Metropolitano Niguarda, Milan, Italy
Background: Antithrombotic treatment, including low molecular weight heparin (LMWH) or unfractionated heparin (UFH), has been proposed as a potential therapy for coronavirus disease 2019 (COVID-19) to lower diffuse intravascular clotting activation. However, it is unclear whether prophylactic or therapeutic doses have similar efficacy in reducing mortality.
Methods: We performed a systematic review (PROSPERO registration CRD42020179955) and meta-analysis including observational cohort studies and randomized controlled trials (RCT) evaluating the effectiveness of heparins (either LMWH, UFH, or fondaparinux) in COVID-19 patients. Heparin treatment was compared to no anticoagulation. A subgroup analysis on prophylactic or therapeutic doses compared to no anticoagulation was performed. Prophylactic dose was also compared to full dose anticoagulation. Primary endpoint was all-cause mortality. Secondary endpoints were major bleeding and length of hospital stay (LOS).
Results: 33 studies (31 observational, 2 RCT) were included for a total overall population of 32,688 patients. Of these, 21,723 (66.5%) were on heparins. 31 studies reported data on all-cause mortality, showing that both prophylactic and full dose reduced mortality (pooled Hazard Ratio [HR] 0.63, 95% confidence interval [CI] 0.57-0.69 and HR 0.56, 95% CI 0.47-0.66, respectively). However, the full dose was associated with a higher risk of major bleeding (Odds Ratio [OR] 2.01, 95% CI 1.14–3.53) compared to prophylactic dose. Finally, LOS was evaluated in 3 studies; no difference was observed between patients with and without heparins (0.98, −3.87, 5.83 days).
Conclusion: Heparin at both full and prophylactic dose is effective in reducing mortality in hospitalized COVID-19 patients, compared to no treatment. However, full dose was associated with an increased risk of bleeding.
Systematic Review Registration: https://clinicaltrials.gov/, identifier CRD42020179955
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing coronavirus disease 2019 (COVID-19) was firstly detected in Wuhan, China, in December 2019 and rapidly spread worldwide with recurrent infection waves. COVID-19 primarily involves the respiratory tract leading, in the more severe cases, to interstitial pneumonia and acute respiratory distress syndrome (ARDS) requiring intensive care unit admission and ventilatory support (Krishnan et al., 2021). Risk factors associated with severe ARDS and poor prognosis are the coexistence of cardiovascular and noncardiovascular comorbidities such as diabetes, hypertension, previous cerebrovascular and cardiovascular disease, chronic obstructive pulmonary disease (COPD), and male sex (Del Sole et al., 2020; Gómez Antúnez et al., 2020; Jordan et al., 2020; Wu et al., 2020; Zhang et al., 2020).
Among pathophysiological mechanisms, it has been shown that COVID-19 may cause a diffuse pulmonary intravascular coagulopathy associated with systemic inflammation promoting an extensive alveolar and interstitial lung inflammation leading to local microthrombosis (McGonagle et al., 2020). COVID-19 may also be implicated in platelet activation and arterial dysfunction leading to arterial thrombosis such as myocardial infarction (Violi et al., 2020). According to these mechanisms, disproportionally high D-dimer levels were also described (Del Sole et al., 2020), which were associated with higher mortality (Soni et al., 2020; Zhang et al., 2020).
Following these observations, empirical treatments targeting inflammatory pathways have been proposed, such as tocilizumab and hydroxychloroquine (Cavalcanti et al., 2020; Ip et al., 2020; Salama et al., 2021), with divergent results among studies (Abubakar et al., 2020; Geleris et al., 2020; Jordan et al., 2020; Lauriola et al., 2020; Abdulrahman et al., 2021; Veiga et al., 2021). Currently, remdesivir is the only recommended drug in virtue of its ability to reduce the length of hospital stay in COVID-19 patients (Beigel et al., 2020).
Besides, therapies aimed at reducing the procoagulant phenotype of these patients, such as low molecular weight heparins (LMWH), have been investigated (Albani et al., 2020; Nadkarni et al., 2020), but the evidence is limited, and guidelines are not completely concordant (Marietta et al., 2020; Moores et al., 2020; Spyropoulos et al., 2020).
However, the real clinical benefit of LMWH in this setting is not known, and it is unclear whether patients should be kept at prophylactic or therapeutic doses of LMWH. For this reason, we conducted a systematic review and meta-analysis of the literature to evaluate the effectiveness of heparin compared to no anticoagulant treatment in reducing overall mortality. Also, we evaluated major bleeding and length of hospital stay in patients treated with heparin as secondary endpoints.
Methods
Searches Strategy and Study Selection
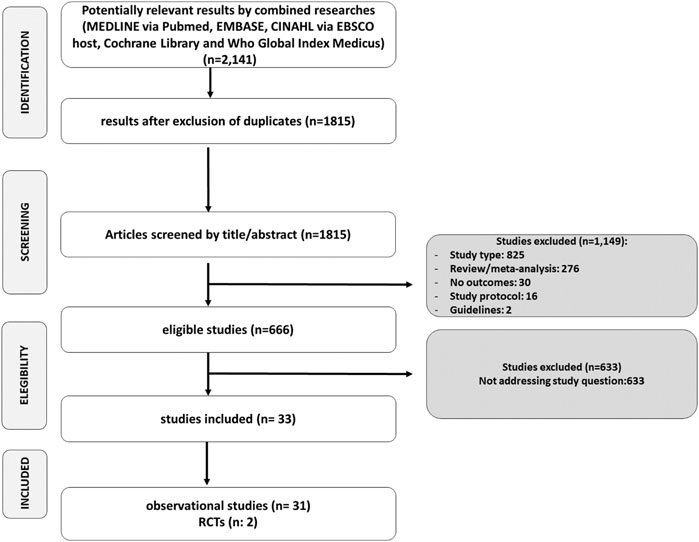
From April 30, 2020, to June 22, 2021, we monthly researched MEDLINE (Pubmed), Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO host), Cochrane Central Register of Controlled Trials (CENTRAL 2020) in the Cochrane Library, and WHO Global Index Medicus for potentially relevant results. The search strategy included “enoxaparin,” “fondaparinux,” and “COVID-19” as keywords and is detailed in Supplementary Material S1. No filters were applied. The search strategy was performed according to PRISMA guidelines. Websites of regulatory agencies and pharmaceutical companies of included treatments were searched, too. We included records in English and Italian.
Initial inclusion criteria were as follows: 1) full-text articles of randomized controlled trials (RCTs) or non-RCT or observational studies; 2) the study condition was COVID-19 in adult patients (older than 18 years); 3) the intervention was enoxaparin or fondaparinux with or without other concomitant therapies for COVID-19 at prophylactic or therapeutic doses; 4) the comparator was placebo or standard of care, with or without other concomitant therapies for COVID-19. Studies administering low molecular weight heparins (LMWH), unfractionated heparin (UFH), or combined anticoagulant regimens with indicated prophylactic or therapeutic dose were included. Studies investigating oral anticoagulants were excluded. Case reports, case series, studies with no comparator, commentaries, and editorials were excluded. Letters were excluded unless reported original data fulfilling our inclusion criteria. Studies without outcomes were excluded. Reviews and meta-analyses were excluded, too.
Retrieved citations were screened by title and abstract independently by six study authors. Full texts of potentially relevant citations were assessed by two authors for final decision of inclusion or exclusion, and disagreements were solved by collegial discussion.
Data Extraction
From the included studies, we collected data on author name, study design, mean age, sex, total patients, treatment and control arms with administered dose, the number of patients in each arm, comorbidities (hypertension, diabetes mellitus, heart failure, and malignancy), setting, D-dimer, and Sequential Organ Failure Assessment (SOFA) score, when available. All studies and outcomes data were collected in an electronic spreadsheet (Microsoft Excel).
Study Outcomes
Included outcomes were all-cause mortality, major bleeding, and length of hospital stay (LoS).
Study Quality and Risk of Bias Assessment
Study quality was evaluated by two study authors (R.G. and D.M.) with Newcastle-Ottawa scales (See Supplementary Table S1). For the evaluation of adequate follow-up in Newcastle-Ottawa scales, we used a threshold of at least 28 days to avoid potential loss of observation of the outcome. Studies with a score ≥7 were considered of good quality. ROBINS-I tool was also used to evaluate the risk of bias of observational studies (Figure 1A; Sterne et al., 2016). RoB2 tool was used to assess risk of bias for RCTs (Figure 1B) (Sterne et al., 2019). Publication bias was evaluated by funnel plots (Supplementary Figure S1).
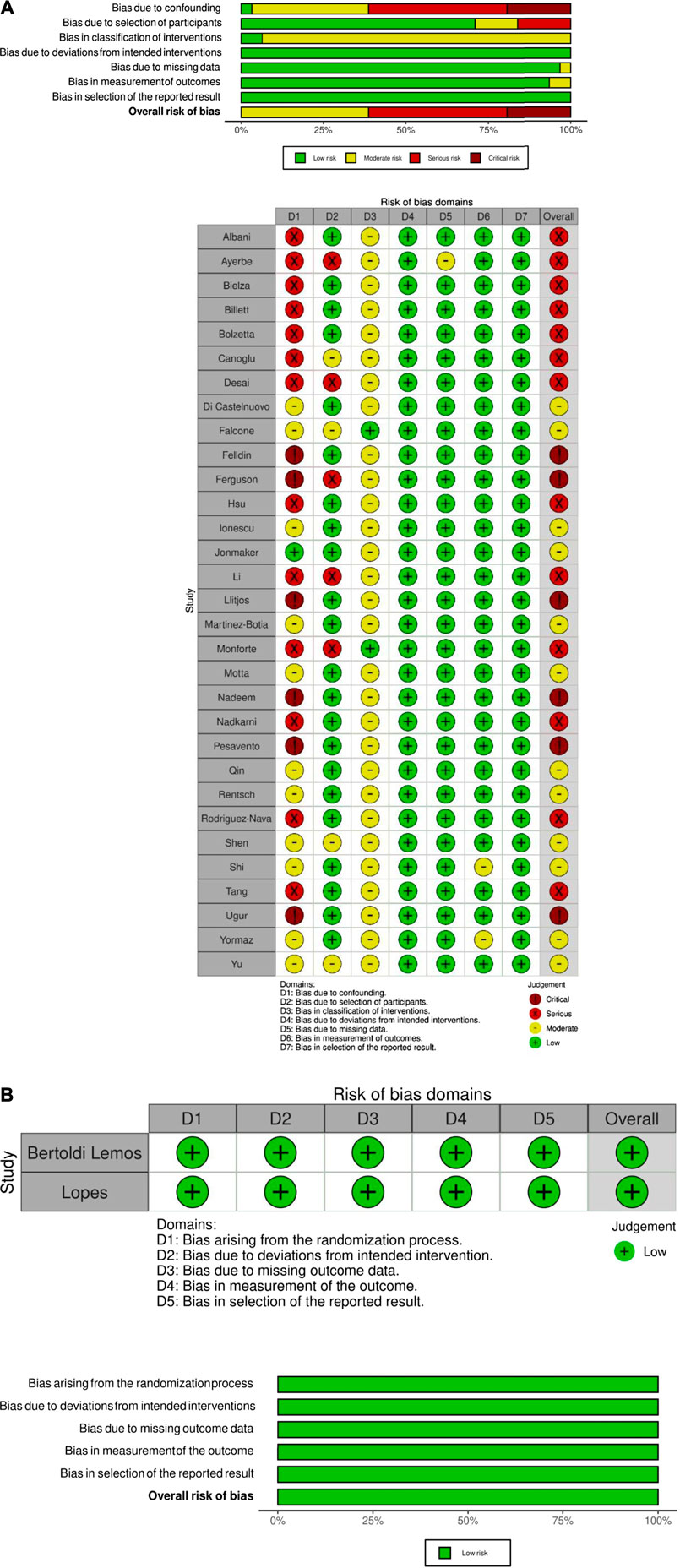
FIGURE 1. Risk of bias assessment of observational studies (Panel A) and randomized controlled trials (Panel B).
Statistical Analyses
A primary analysis was performed on all included studies on the basis of prophylactic, full dose, and overall treatment with enoxaparin, fondaparinux, an unspecified LMWH, UFH, or combined anticoagulant regimens compared to placebo or standard of care. Also, a comparison between prophylactic and full dose treatment was performed. For studies not reporting HR estimates, when sufficient other information was available, effects and their standard errors were approximated as described in Tierney et al. (2007). Odds ratios (OR) and their standard errors were directly calculated on the basis of the number of subjects and events per group. Meta-analyses for each endpoint separately were performed based on random effect models, using the logarithm of hazard ratios (HR) or OR as outcome. According to Higgins et al. (2009), we performed Bayesian meta-analysis with informative priors, since some analyses were based on a limited number of studies. For the LoS endpoint, we performed a meta-analysis of differences in medians, rather than in means, according to McGrath et al. (2020). Evaluation of the difference in medians is here more appropriate for two reasons: first, many studies only report information on quantiles (e.g., median and quartiles), and mapping to mean and standard deviation might be biased; secondly, LoS is skewed, and, therefore, the median is a more appropriate summary. Analyses were performed using the R software (R Development Core Team, 2018) version 3.5.1.
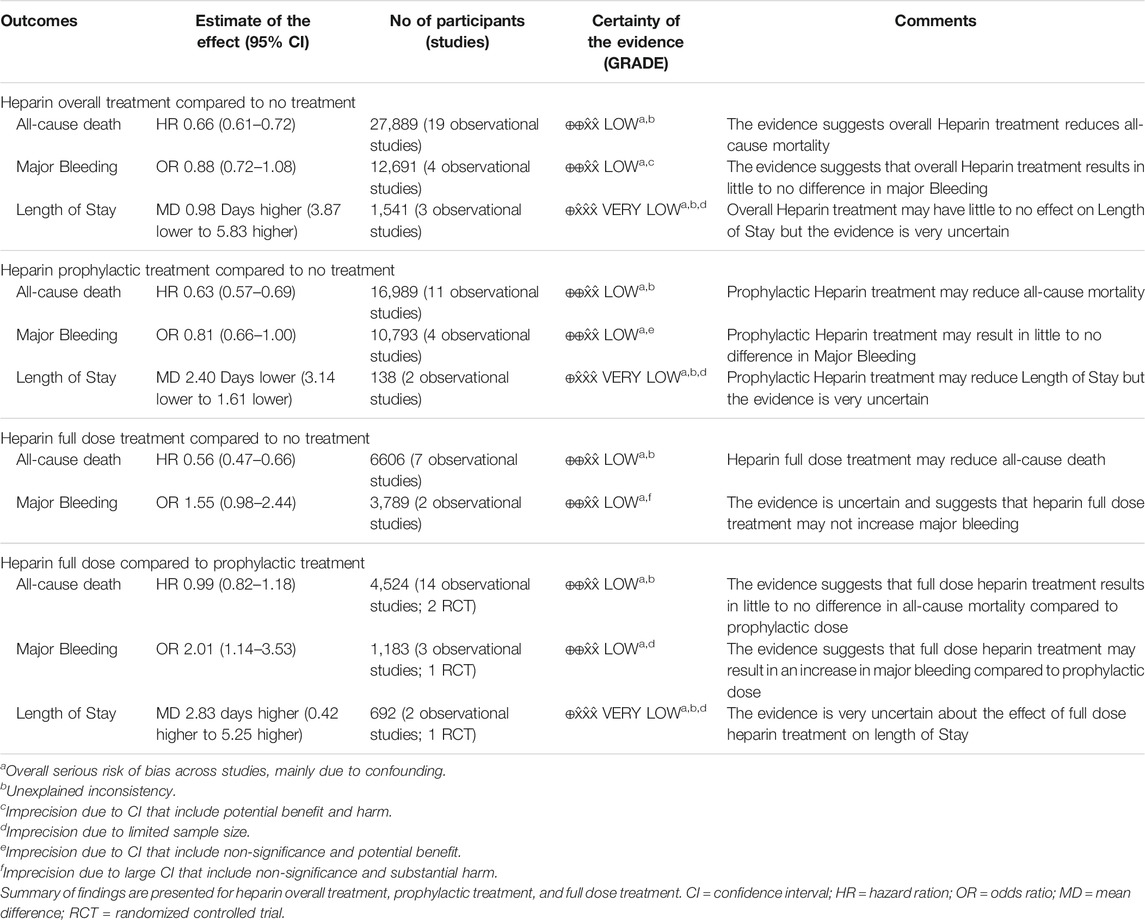
Summary of Findings
Summary of findings with grading of the quality of the evidence was performed using GRADEproGDT according to the GRADE Handbook by two study authors (Zhang et al., 2020). Discrepancies were resolved by discussion.
Study Registration and Approval
This study was registered in PROSPERO (CRD42020179955). Due to the secondary nature of the study on already published data, institutional review board (IRB) approval and patient consent were not necessary.
Results
Study Characteristics and Results of Individual Studies
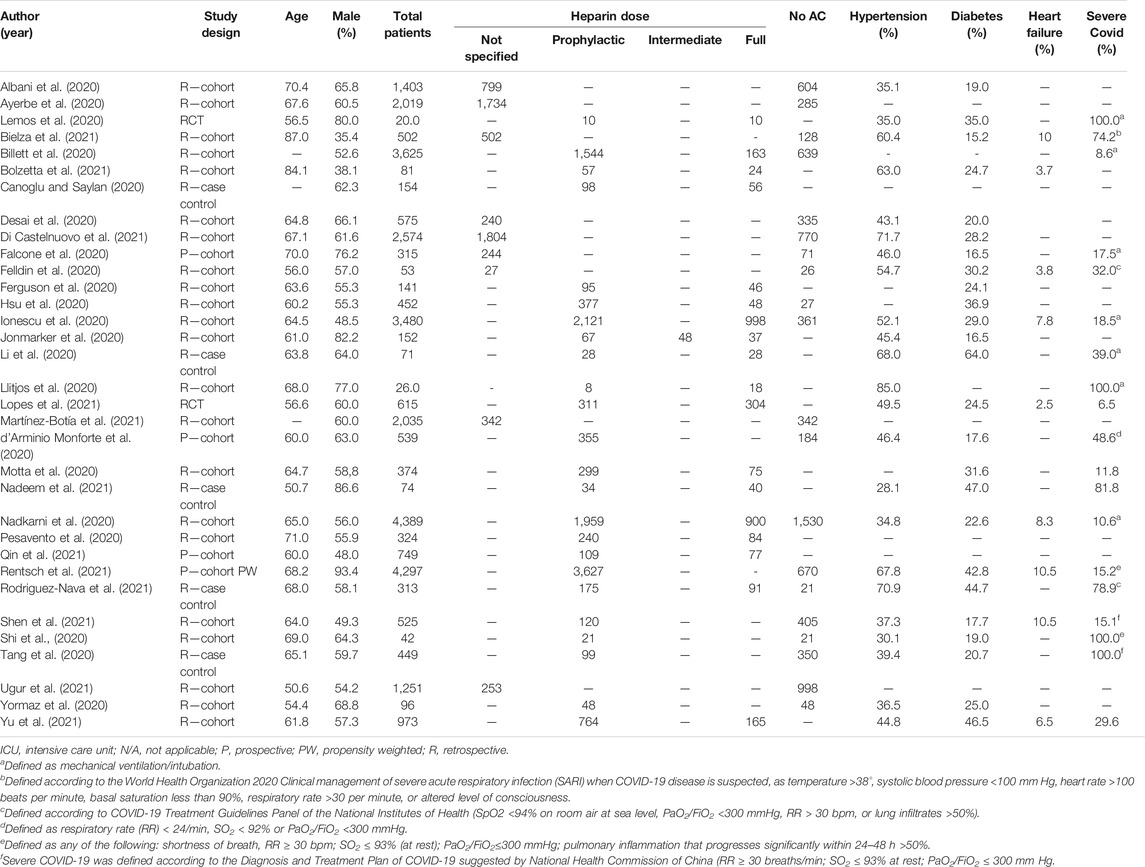
After screening, 666 potentially eligible studies were identified and were considered for detailed analysis (Figure 2); 33 studies were finally included in the meta-analysis: 31 observational studies and 2 RCTs. Included studies’ characteristics are detailed in Table 1.
Quality assessment showed a general low quality of observational studies, with only five studies included having a score ≥7 (Figure 1; Supplementary Table S1).
A total of 32,688 patients with COVID-19 were included, of whom 21,723 (66.5%) were on treatment with heparins (including LMWH and UFH) or fondaparinux, and 10,965 (33.5%) were not treated with anticoagulants. Men were the most represented with the prevalence ranging from 35.4% to 80.0% among studies, while the range of age among studies was 55.0–87.0 years. The rate of patients with hypertension and diabetes ranges among 28.1–85.0% and 15.2–64.0%, respectively. The proportion of patients with severe COVID-19 ranged between 6.5 and 100%.
The use of heparins was highly heterogeneous, and a detailed definition of treatments for each included study is reported in Supplementary Table S2.
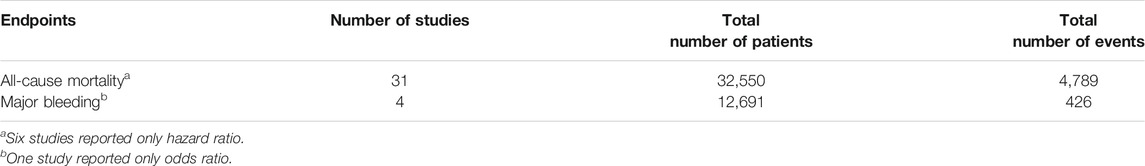
All-Cause Mortality
Overall, 31 studies reported data on all-cause mortality including 32,550 patients and 4,789 deaths (Table 2).
In the overall analysis (Figure 3A), heparin treatment reduced the risk of all-cause mortality (pooled HR 0.66, 95% CI 0.61–0.72). These results were confirmed by sensitivity analysis performed on both prophylactic (Figure 3B) and full dose of heparin (Figure 3C) (pooled HR 0.63, 95% CI 0.57–0.69 and pooled HR 0.56, 95% CI 0.47–0.66, respectively).
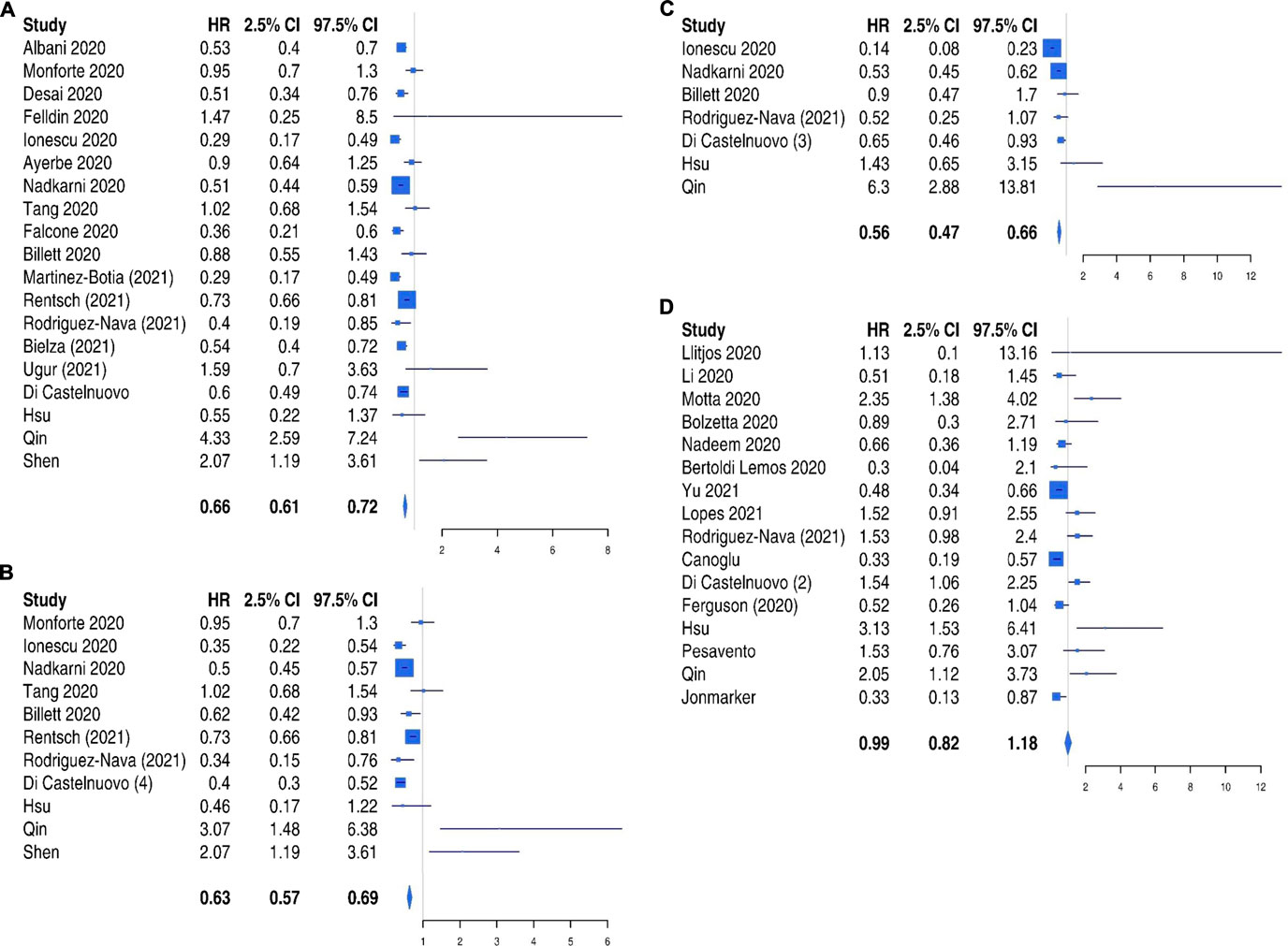
FIGURE 3. All-cause mortality risk in patients treated with heparin: overall analysis (Panel A), prophylactic dose (Panel B), and full dose (Panel C) compared to no treatment and comparison between full dose and prophylactic dose (Panel D).
Furthermore, a direct comparison of full and prophylactic dose (Figure 3D) was performed, and no difference was found between the two strategies in the reduction of mortality (HR 0.99, 95% CI 0.82–1.18).
Major Bleeding
Four studies reported data on major bleeding including 12,691 patients and 426 MBs (Table 2). In the overall analysis (Supplementary Figure S2A), no difference was observed regarding the occurrence of major bleeding in patients treated or not with heparin (Odds Ratio [OR] 0.88, 95% CI 0.77–1.08). Both prophylactic (Supplementary Figure S2B) and full dose (Supplementary Figure S2C) of heparin did not significantly increase bleeding risk when compared to no treatment (OR 0.81, 95% CI 0.66–1.0 and OR 1.55, 95% CI 0.98–2.44, respectively). A full dose was associated with an increased risk of bleeding compared to prophylactic (OR 2.01, 95% CI 1.14–3.53) (Supplementary Figure S2D).
Length of Hospital Stay
Six studies reported data on length of hospital stay including 2,233 patients, of whom 1,056 were not treated with heparin. The difference of length of stay for all heparin treatment compared to no treatment (Supplementary Figure S3A) was 0.98 (−3.87, 5.83), while prophylactic dose reduced the length of stay compared to no treatment (Supplementary Figure S3B) (−2.38, −3.14, −1.61). A full dose was associated with higher length of stay compared to prophylactic dose (2.83, 0.42, and 5.25).
A summary of pooled results of meta-analysis according to each endpoint are shown in Figure 2, and a summary of findings according to GRADE guidelines is reported in Table 3.
Discussion
The main finding of our meta-analysis is that heparin treatment (either enoxaparin, other LMWH, or UFH) significantly reduced in-hospital mortality in COVID-19 patients. We found that both prophylactic and therapeutic doses of heparin were similarly associated with a reduced mortality, with the advantage of a lower bleeding risk in the group of patients treated with prophylactic dose.
Given the similar effectiveness profile, our data does not support an extensive use of full-dose anticoagulation in all hospitalized COVID-19 patients and suggests that prophylactic dose should represent the first-choice treatment, especially in patients with high bleeding risk.
Our study showed no difference in overall mortality between prophylactic and full dose of anticoagulation. This evidence is consistent with National Institutes of Health (NIH) guidelines (Hindricks et al., 2021), which suggest that a prophylactic dose of anticoagulants should be administered to hospitalized patients with SARS-CoV-2 infection unless contraindicated (level of evidence AIII), preferring LMWH over oral anticoagulants. In addition, NIH guidelines do not support the use of therapeutic dose of antithrombotic treatment due to lack of evidence (Hindricks et al., 2021). Our study confirms the beneficial effect of prophylactic LMWH in reducing all-cause mortality which should be preferred to therapeutic LMWH filling up current NIH guidelines. Also, CHEST guidelines recommend the use of a prophylactic dose of heparins over intermediate and therapeutic dose of heparins in severely ill patients with COVID-19 (Moores et al., 2020). Of note, CHEST guidelines support the use of LMWH or fondaparinux over UFH, and the use of heparins over direct oral anticoagulants (Moores et al., 2020).
Recently, the World Health Organization (WHO) guidelines suggested the use of prophylactic over therapeutic LMWH given the very low evidence on therapeutic LMWH in lowering mortality and pulmonary embolism, along with an increased risk of major bleedings (Jakobsen et al., 2019).
The studies included in our analysis had a variable proportion of severe COVID-19, suggesting that LMWH administration may be useful in patients with both mild/moderate and severe COVID-19. This finding is consistent with the International Society of Thrombosis and Haemostasis (ISTH) interim guidance, which suggests that the use of LMWH should be used in all hospitalized COVID-19 patients (Thachil et al., 2020).
However, it is reassuring that heparin treatment was not globally associated with an increased risk of major bleeding, suggesting that it can be safely administered in this clinical setting. Nevertheless, this analysis was performed on a limited number of patients and cannot be considered as definitive. According to our findings, the American Society of Hematology (ASH) recently suggested the use prophylactic-intensity over intermediate and therapeutic-intensity anticoagulation in patients with COVID-19-related acute illness without established or suspected VTE, but this recommendation was based on very low certainty of evidence (Cuker et al., 2021).
Three clinical trials, the Randomized, Embedded, Multi-factorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP, NCT02735707) Therapeutic Anticoagulation, Accelerating COVID-19 Therapeutic Interventions and Vaccines-4 (ACTIV-4, NCT04505774) Antithrombotics Inpatient, and Antithrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC, NCT04372589), are ongoing, and partial results were available in a press release, which reported an interim analysis on 1000 COVID-19 patients (Cuker et al., 2021; National Institutes of Health, 2021), showing that full-dose anticoagulation in patients with moderate COVID-19, as defined by patients who did not need mechanical ventilation or intensive care unit admission, seems to reduce the need for mechanical ventilation or other supportive interventions, with similar safety than prophylactic dose (National Institutes of Health, 2021).
As a secondary endpoint, we analyzed the association between heparin use and length of stay. We found that a prophylactic dose of heparin seemed to reduce length of stay: this may be caused by the clinical choice of higher over prophylactic doses in patients with severe illness or admitted in intensive care unit. Indeed, in the included studies, this choice was often based on disease severity, with severe patients receiving more frequently the full dose anticoagulation.
There are still some open issues not assessed in this study, such as the case whether the administration of oral anticoagulants may be as effective as the subcutaneous/intravenous one in these patients. Furthermore, we do not know if a D-dimer-based strategy guiding the dose of heparin may be more effective than a standard weight-adjusted prophylactic dose. There are also some patients experiencing acute renal failure or liver enzymes elevation during the in-hospital staying (Lei et al., 2020); thus, the effectiveness and safety of heparin in these high-risk patients should be confirmed.
Study Limitations
Our study has some limitations. First, fondaparinux was not well represented among studies, so that these results cannot be applied to this drug with certainty. In addition, in two studies (Ionescu et al., 2020; Nadkarni et al., 2020), a small number of patients were treated with apixaban, an oral inhibitor of Xa factor, which has the same target of heparin, possibly representing a potential confounding factor.
Moreover, the quality of studies was generally unsatisfactory, with only 11 studies included having a score ≥7 in the Newcastle-Ottawa scale evaluation. The risk of bias, assessed with ROBINS-I tool, showed an overall serious risk of bias, especially due to confounding. Furthermore, very different regimens of heparin treatments were adopted.
Another aspect relates to the effectiveness of heparin according to COVID-19 severity; indeed, the proportion of severe patients was highly variable among studies, and this may affect the overall results. Further study in severe patients is needed.
Furthermore, the rationale for treatment assignment was not univocal across studies and included disease severity, D-dimer levels, and physician choice. D-dimer levels were expressed only in a limited number of studies and with high variability in the unit of measurement used. For this reason, we could not use D-dimer levels for further analyses.
Conclusion
In conclusion, our results indicate that heparin is effective in reducing all-cause mortality in hospitalized COVID-19 patients compared to no treatment. We did not find a clear advantage of using therapeutic over prophylactic dose of heparin, along with an increased bleeding risk in patients treated with full dose heparin.
Data Availability Statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Author Contributions
RG and DM contributed to the study conception and design, data acquisition, analysis and interpretation, and paper drafting. AP contributed to the study conception, data interpretation, and paper drafting. ET, AR, RR, AN, PS, and ED contributed to the data acquisition and analysis. VF contributed to the study design and data acquisition. AF performed the statistical analyses and contributed to paper drafting and critical revision. FS and DP contributed to study conception and design, paper drafting and gave a critical revision for intellectual content.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2021.698008/full#supplementary-material
References
Abdulrahman, A., AlSayed, I., AlMadhi, M., AlArayed, J., Mohammed, S. J., Sharif, A. K., et al. (2021). The Efficacy and Safety of Hydroxychloroquine in Patients with COVID-19: A Multicenter National Retrospective Cohort. Infect. Dis. Ther. 10, 439. doi:10.1007/s40121-021-00397-8
Abubakar, A. R., Sani, I. H., Godman, B., Kumar, S., Islam, S., Jahan, I., et al. (2020). Systematic Review on the Therapeutic Options for COVID-19: Clinical Evidence of Drug Efficacy and Implications. Infect. Drug Resist. 13, 4673–4695. doi:10.2147/IDR.S289037
Albani, F., Sepe, L., Fusina, F., Prezioso, C., Baronio, M., Caminiti, F., et al. (2020). Thromboprophylaxis with Enoxaparin Is Associated with a Lower Death Rate in Patients Hospitalized with SARS-CoV-2 Infection. A Cohort Study. EClinicalMedicine 27, 100562. doi:10.1016/j.eclinm.2020.100562
Ayerbe, L., Risco, C., and Ayis, S. (2020). The Association between Treatment with Heparin and Survival in Patients with Covid-19. J. Thromb. Thrombolysis 50 (2), 298–301. doi:10.1007/s11239-020-02162-z
Beigel, J. H., Tomashek, K. M., Dodd, L. E., Mehta, A. K., Zingman, B. S., Kalil, A. C., et al. (2020). Remdesivir for the Treatment of Covid-19 - Final Report. N. Engl. J. Med. 383 (19), 1813–1826. doi:10.1056/NEJMoa2007764
Bielza, R., Sanz, J., Zambrana, F., Arias, E., Malmierca, E., Portillo, L., et al. (2021). Clinical Characteristics, Frailty, and Mortality of Residents with COVID-19 in Nursing Homes of a Region of Madrid. J. Am. Med. Dir. Assoc. 22 (2), 245–e2. doi:10.1016/j.jamda.2020.12.003
Billett, H. H., Reyes-Gil, M., Szymanski, J., Ikemura, K., Stahl, L. R., Lo, Y., et al. (2020). Anticoagulation in COVID-19: Effect of Enoxaparin, Heparin, and Apixaban on Mortality. Thromb. Haemost. 120 (12), 1691–1699. doi:10.1055/s-0040-1720978
Bolzetta, F., Maselli, M., Formilan, M., Busonera, F., Albanese, P., Chiaromanni, F., et al. (2021). Prophylactic or Therapeutic Doses of Heparins for COVID-19 Infection? A Retrospective Study. Aging Clin. Exp. Res. 33 (1), 213–217. doi:10.1007/s40520-020-01750-6
Canoglu, K., and Saylan, B. (2020). Therapeutic Dosing of Low-Molecular-Weight Heparin May Decrease Mortality in Patients with Severe COVID-19 Infection. Ann. Saudi Med. 40 (6), 462–468. doi:10.5144/0256-4947.2020.462
Cavalcanti, A. B., Zampieri, F. G., Rosa, R. G., Azevedo, L. C. P., Veiga, V. C., Avezum, A., et al. (2020). Hydroxychloroquine with or without Azithromycin in Mild-To-Moderate Covid-19. N. Engl. J. Med. 383 (21), 2041–2052. doi:10.1056/NEJMoa2019014
Cuker, A., Tseng, E. K., Nieuwlaat, R., Angchaisuksiri, P., Blair, C., Dane, K., et al. (2021). American Society of Hematology 2021 Guidelines on the Use of Anticoagulation for Thromboprophylaxis in Patients with COVID-19. Blood Adv. 5 (3), 872–888. doi:10.1182/bloodadvances.2020003763
d'Arminio Monforte, A., Tavelli, A., Bai, F., Tomasoni, D., Falcinella, C., Castoldi, R., et al. (2020). The Importance of Patients' Case-Mix for the Correct Interpretation of the Hospital Fatality Rate in COVID-19 Disease. Int. J. Infect. Dis. 100, 67–74. doi:10.1016/j.ijid.2020.09.037
Del Sole, F., Farcomeni, A., Loffredo, L., Carnevale, R., Menichelli, D., Vicario, T., et al. (2020). Features of Severe COVID-19: A Systematic Review and Meta-Analysis. Eur. J. Clin. Invest. 50 (10), e13378. doi:10.1111/eci.13378
Desai, A., Voza, G., Paiardi, S., Teofilo, F. I., Caltagirone, G., Pons, M. R., et al. (2020). The Role of Anti-hypertensive Treatment, Comorbidities and Early Introduction of LMWH in the Setting of COVID-19: A Retrospective, Observational Study in Northern Italy. Int. J. Cardiol. 324, 249. doi:10.1016/j.ijcard.2020.09.062
Di Castelnuovo, A., Costanzo, S., Antinori, A., Berselli, N., Blandi, L., Bonaccio, M., et al. (2021). Heparin in COVID-19 Patients Is Associated with Reduced In-Hospital Mortality: the Multicenter Italian CORIST Study. Thromb. Haemost. 121, 1054–1065. doi:10.1055/a-1347-6070
Falcone, M., Tiseo, G., Barbieri, G., Galfo, V., Russo, A., Virdis, A., et al. (2020). Role of Low-Molecular-Weight Heparin in Hospitalized Patients with Severe Acute Respiratory Syndrome Coronavirus 2 Pneumonia: A Prospective Observational Study. Open Forum Infect. Dis. 7 (12), ofaa563. doi:10.1093/ofid/ofaa563
Felldin, M., Søfteland, J. M., Magnusson, J., Ekberg, J., Karason, K., Schult, A., et al. (2020). Initial Report from a Swedish High-Volume Transplant Center after the First Wave of the COVID-19 Pandemic. Transplantation 105, 108. doi:10.1097/TP.0000000000003436
Ferguson, J., Volk, S., Vondracek, T., Flanigan, J., and Chernaik, A. (2020). Empiric Therapeutic Anticoagulation and Mortality in Critically Ill Patients with Respiratory Failure from SARS-CoV-2: A Retrospective Cohort Study. J. Clin. Pharmacol. 60 (11), 1411–1415. doi:10.1002/jcph.1749
Geleris, J., Sun, Y., Platt, J., Zucker, J., Baldwin, M., Hripcsak, G., et al. (2020). Observational Study of Hydroxychloroquine in Hospitalized Patients with Covid-19. N. Engl. J. Med. 382 (25), 2411–2418. doi:10.1056/NEJMoa2012410
Gómez Antúnez, M., Muiño Míguez, A., Bendala Estrada, A. D., Maestro de la Calle, G., Monge Monge, D., Boixeda, R., et al. (2020). Clinical Characteristics and Prognosis of COPD Patients Hospitalized with SARS-CoV-2. Int. J. Chron. Obstruct Pulmon Dis. 15, 3433–3445. doi:10.2147/COPD.S276692
Higgins, J. P., Thompson, S. G., and Spiegelhalter, D. J. (2009). A Re-evaluation of Random-Effects Meta-Analysis. J. R. Stat. Soc. Ser. A. Stat. Soc. 172 (1), 137–159. doi:10.1111/j.1467-985X.2008.00552.x
Hindricks, G., Potpara, T., Dagres, N., Arbelo, E., Bax, J. J., Blomström-Lundqvist, C., et al. (2021). 2020 ESC Guidelines for the Diagnosis and Management of Atrial Fibrillation Developed in Collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 42 (5), 373–498. doi:10.1093/eurheartj/ehaa612
Hsu, A., Liu, Y., Zayac, A. S., Olszewski, A. J., and Reagan, J. L. (2020). Intensity of Anticoagulation and Survival in Patients Hospitalized with COVID-19 Pneumonia. Thromb. Res. 196, 375–378. doi:10.1016/j.thromres.2020.09.030
Ionescu, F., Jaiyesimi, I., Petrescu, I., Lawler, P. R., Castillo, E., Munoz-Maldonado, Y., et al. (2020). Association of Anticoagulation Dose and Survival in Hospitalized COVID-19 Patients: A Retrospective Propensity Score-Weighted Analysis. Eur. J. Haematol. 106, 165. doi:10.1111/ejh.13533
Ip, A., Berry, D. A., Hansen, E., Goy, A. H., Pecora, A. L., Sinclaire, B. A., et al. (2020). Hydroxychloroquine and Tocilizumab Therapy in COVID-19 Patients-An Observational Study. PLoS One 15 (8), e0237693. doi:10.1371/journal.pone.0237693
Jakobsen, C. B., Lamberts, M., Carlson, N., Lock-Hansen, M., Torp-Pedersen, C., Gislason, G. H., et al. (2019). Incidence of Atrial Fibrillation in Different Major Cancer Subtypes: a Nationwide Population-Based 12 Year Follow up Study. BMC Cancer 19 (1), 1105. doi:10.1186/s12885-019-6314-9
Jonmarker, S., Hollenberg, J., Dahlberg, M., Stackelberg, O., Litorell, J., Everhov, Å. H., et al. (2020). Dosing of Thromboprophylaxis and Mortality in Critically Ill COVID-19 Patients. Crit. Care 24 (1), 653. doi:10.1186/s13054-020-03375-7
Jordan, R. E., Adab, P., and Cheng, K. K. (2020). Covid-19: Risk Factors for Severe Disease and Death. BMJ 368, m1198. doi:10.1136/bmj.m1198
Krishnan, A., Hamilton, J. P., Alqahtani, S. A., and Woreta, T. A. (2021). A Narrative Review of Coronavirus Disease 2019 (COVID-19): Clinical, Epidemiological Characteristics, and Systemic Manifestations. Intern. Emerg. Med. 16, 815. doi:10.1007/s11739-020-02616-5
Lauriola, M., Pani, A., Ippoliti, G., Mortara, A., Milighetti, S., Mazen, M., et al. (2020). Effect of Combination Therapy of Hydroxychloroquine and Azithromycin on Mortality in Patients with COVID-19. Clin. Transl Sci. 13 (6), 1071–1076. doi:10.1111/cts.12860
Lei, F., Liu, Y. M., Zhou, F., Qin, J. J., Zhang, P., Zhu, L., et al. (2020). Longitudinal Association between Markers of Liver Injury and Mortality in COVID-19 in China. Hepatology 72 (2), 389–398. doi:10.1002/hep.31301
Lemos, A. C. B., do Espírito Santo, D. A., Salvetti, M. C., Gilio, R. N., Agra, L. B., Pazin-Filho, A., et al. (2020). Therapeutic versus Prophylactic Anticoagulation for Severe COVID-19: A Randomized Phase II Clinical Trial (HESACOVID). Thromb. Res. 196, 359–366. doi:10.1016/j.thromres.2020.09.026
Li, M. G. S., Nyabera, A., Kondaveeti, R., Hammudeh, Y., Gonzalez, C., Trandafirescu, T., et al. (2020). Continuous Infusion Low-Dose Unfractionated Heparin for the Management of Hypercoagulability Associated with COVID-19. J. Pharm. Pract. doi:10.1177/0897190020966207
Llitjos, J. F., Leclerc, M., Chochois, C., Monsallier, J. M., Ramakers, M., Auvray, M., et al. (2020). High Incidence of Venous Thromboembolic Events in Anticoagulated Severe COVID-19 Patients. J. Thromb. Haemost. 18 (7), 1743–1746. doi:10.1111/jth.14869
Lopes, R. D., de Barros E Silva, P. G. M., Furtado, R. H. M., Macedo, A. V. S., Bronhara, B., Damiani, L. P., et al. (2021). Therapeutic versus Prophylactic Anticoagulation for Patients Admitted to Hospital with COVID-19 and Elevated D-Dimer Concentration (ACTION): an Open-Label, Multicentre, Randomised, Controlled Trial. Lancet 397 (10291), 2253–2263. doi:10.1016/S0140-6736(21)01203-4
Marietta, M., Ageno, W., Artoni, A., De Candia, E., Gresele, P., Marchetti, M., et al. (2020). COVID-19 and Haemostasis: a Position Paper from Italian Society on Thrombosis and Haemostasis (SISET). Blood Transfus. 18 (3), 167–169. doi:10.2450/2020.0083-20
Martínez-Botía, P., Bernardo, Á., Acebes-Huerta, A., Caro, A., Leoz, B., Martínez-Carballeira, D., et al. (2021). Clinical Management of Hypertension, Inflammation and Thrombosis in Hospitalized COVID-19 Patients: Impact on Survival and Concerns. J. Clin. Med. 10 (5), 1073. doi:10.3390/jcm10051073
McGonagle, D., O'Donnell, J. S., Sharif, K., Emery, P., and Bridgewood, C. (2020). Immune Mechanisms of Pulmonary Intravascular Coagulopathy in COVID-19 Pneumonia. Lancet Rheumatol. 2 (7), e437–e445. doi:10.1016/S2665-9913(20)30121-1
McGrath, S., Sohn, H., Steele, R., and Benedetti, A. (2020). Meta-analysis of the Difference of Medians. Biom J. 62 (1), 69–98. doi:10.1002/bimj.201900036
Moores, L. K., Tritschler, T., Brosnahan, S., Carrier, M., Collen, J. F., Doerschug, K., et al. (2020). Prevention, Diagnosis, and Treatment of VTE in Patients with Coronavirus Disease 2019: CHEST Guideline and Expert Panel Report. Chest 158 (3), 1143–1163. doi:10.1016/j.chest.2020.05.559
Motta, J. K., Ogunnaike, R. O., Shah, R., Stroever, S., Cedeño, H. V., Thapa, S. K., et al. (2020). Clinical Outcomes with the Use of Prophylactic versus Therapeutic Anticoagulation in Coronavirus Disease 2019. Crit. Care Explor 2 (12), e0309. doi:10.1097/CCE.0000000000000309
Nadeem, R., Thomas, S. J., Fathima, Z., Palathinkal, A. S., Alkilani, Y. E., Dejan, E. A., et al. (2021). Pattern of Anticoagulation Prescription for Patients with Covid-19 Acute Respiratory Distress Syndrome Admitted to ICU. Does it Impact Outcome? Heart Lung 50 (1), 1–5. doi:10.1016/j.hrtlng.2020.10.009
Nadkarni, G. N., Lala, A., Bagiella, E., Chang, H. L., Moreno, P. R., Pujadas, E., et al. (2020). Anticoagulation, Bleeding, Mortality, and Pathology in Hospitalized Patients with COVID-19. J. Am. Coll. Cardiol. 76 (16), 1815–1826. doi:10.1016/j.jacc.2020.08.041
National Institutes of Health (2021). Full-dose Blood Thinners Decreased Need for Life Support and Improved Outcome in Hospitalized COVID-19 Patients. Available at: https://www.nih.gov/news-events/news-releases/full-dose-blood-thinners-decreased-need-life-support-improved-outcome-hospitalized-covid-19-patients (Accessed January 22, 2021).
Pesavento, R., Ceccato, D., Pasquetto, G., Monticelli, J., Leone, L., Frigo, A., et al. (2020). The hazard of (Sub)therapeutic Doses of Anticoagulants in Non-critically Ill Patients with Covid-19: The Padua Province Experience. J. Thromb. Haemost. 18 (10), 2629–2635. doi:10.1111/jth.15022
Qin, W., Dong, F., Zhang, Z., Hu, B., Chen, S., Zhu, Z., et al. (2021). Low Molecular Weight Heparin and 28-day Mortality Among Patients with Coronavirus Disease 2019: A Cohort Study in the Early Epidemic Era. Thromb. Res. 198, 19–22. doi:10.1016/j.thromres.2020.11.020
Rentsch, C. T., Beckman, J. A., Tomlinson, L., Gellad, W. F., Alcorn, C., Kidwai-Khan, F., et al. (2021). Early Initiation of Prophylactic Anticoagulation for Prevention of Coronavirus Disease 2019 Mortality in Patients Admitted to Hospital in the United States: Cohort Study. BMJ 372, n311. doi:10.1136/bmj.n311
Rodriguez-Nava, G., Yanez-Bello, M. A., Trelles-Garcia, D. P., Chung, C. W., Chaudry, S., Khan, A. S., et al. (2021). Clinical Characteristics and Risk Factors for Death of Hospitalized Patients with COVID-19 in a Community Hospital: A Retrospective Cohort Study. Mayo Clin. Proc. Innov. Qual. Outcomes 5 (1), 1–10. doi:10.1016/j.mayocpiqo.2020.10.007
Salama, C., Han, J., Yau, L., Reiss, W. G., Kramer, B., Neidhart, J. D., et al. (2021). Tocilizumab in Patients Hospitalized with Covid-19 Pneumonia. N. Engl. J. Med. 384 (1), 20–30. doi:10.1056/NEJMoa2030340
Shen, L., Qiu, L., Liu, D., Wang, L., Huang, H., Ge, H., et al. (2021). The Association of Low Molecular Weight Heparin Use and In-Hospital Mortality Among Patients Hospitalized with COVID-19. Cardiovasc. Drugs Ther. doi:10.1007/s10557-020-07133-3
Shi, C., Wang, C., Wang, H., Yang, C., Cai, F., Zeng, F., et al. (2020). The Potential of Low Molecular Weight Heparin to Mitigate Cytokine Storm in Severe COVID-19 Patients: A Retrospective Cohort Study. Clin. Transl Sci. 13 (6), 1087–1095. doi:10.1111/cts.12880
Soni, M., Gopalakrishnan, R., Vaishya, R., and Prabu, P. (2020). D-dimer Level Is a Useful Predictor for Mortality in Patients with COVID-19: Analysis of 483 Cases. Diabetes Metab. Syndr. 14 (6), 2245–2249. doi:10.1016/j.dsx.2020.11.007
Spyropoulos, A. C., Levy, J. H., Ageno, W., Connors, J. M., Hunt, B. J., Iba, T., et al. (2020). Scientific and Standardization Committee Communication: Clinical Guidance on the Diagnosis, Prevention, and Treatment of Venous Thromboembolism in Hospitalized Patients with COVID-19. J. Thromb. Haemost. 18 (8), 1859–1865. doi:10.1111/jth.14929
Sterne, J. A., Hernán, M. A., Reeves, B. C., Savović, J., Berkman, N. D., Viswanathan, M., et al. (2016). ROBINS-I: a Tool for Assessing Risk of Bias in Non-randomised Studies of Interventions. BMJ 355, i4919. doi:10.1136/bmj.i4919
Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., et al. (2019). RoB 2: a Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 366, l4898. doi:10.1136/bmj.l4898
Tang, N., Bai, H., Chen, X., Gong, J., Li, D., and Sun, Z. (2020). Anticoagulant Treatment Is Associated with Decreased Mortality in Severe Coronavirus Disease 2019 Patients with Coagulopathy. J. Thromb. Haemost. 18 (5), 1094–1099. doi:10.1111/jth.14817
Thachil, J., Tang, N., Gando, S., Falanga, A., Cattaneo, M., Levi, M., et al. (2020). ISTH Interim Guidance on Recognition and Management of Coagulopathy in COVID-19. J. Thromb. Haemost. 18 (5), 1023–1026. doi:10.1111/jth.14810
Tierney, J. F., Stewart, L. A., Ghersi, D., Burdett, S., and Sydes, M. R. (2007). Practical Methods for Incorporating Summary Time-To-Event Data into Meta-Analysis. Trials 8, 16. doi:10.1186/1745-6215-8-16
Ugur, M., Adiyeke, E., Recep, E., Bakan, N., and Yiyit, N. (2021). Aggressive Thromboprophylaxis Improves Clinical Process and Decreases the Need of Intensive Care Unit in Covid-19. Pak J. Med. Sci. 37 (3), 668–674. doi:10.12669/pjms.37.3.3687
Veiga, V. C., Prats, J. A. G. G., Farias, D. L. C., Rosa, R. G., Dourado, L. K., Zampieri, F. G., et al. (2021). Effect of Tocilizumab on Clinical Outcomes at 15 Days in Patients with Severe or Critical Coronavirus Disease 2019: Randomised Controlled Trial. BMJ 372, n84. doi:10.1136/bmj.n84
Violi, F., Pastori, D., Cangemi, R., Pignatelli, P., and Loffredo, L. (2020). Hypercoagulation and Antithrombotic Treatment in Coronavirus 2019: A New Challenge. Thromb. Haemost. 120 (6), 949–956. doi:10.1055/s-0040-1710317
Wu, C., Chen, X., Cai, Y., Xia, J., Zhou, X., Xu, S., et al. (2020). Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 180 (7), 934–943. doi:10.1001/jamainternmed.2020.0994
Yormaz, B., ErgUn, D., Tu, B., ErgUn, R., Arslan, U., and Kanat, F. (2020). The Impact of the "low Molecular Weight Heparin" Administration on the Clinical Course of COVID-19 Disease. Turk J. Med. Sci.
Yu, B., Gutierrez, V. P., Carlos, A., Hoge, G., Pillai, A., Kelly, J. D., et al. (2021). Empiric Use of Anticoagulation in Hospitalized Patients with COVID-19: a Propensity Score-Matched Study of Risks and Benefits. Biomark Res. 9 (1), 29. doi:10.1186/s40364-021-00283-y
Zhang, J., Wang, X., Jia, X., Li, J., Hu, K., Chen, G., et al. (2020). Risk Factors for Disease Severity, Unimprovement, and Mortality in COVID-19 Patients in Wuhan, China. Clin. Microbiol. Infect. 26 (6), 767–772. doi:10.1016/j.cmi.2020.04.012
Keywords: SARS-CoV2, COVID-19, mortality, heparin, LMWH, bleeding, thromboembolism
Citation: Giossi R, Menichelli D, Pani A, Tratta E, Romandini A, Roncato R, Nani A, Schenardi P, Diani E, Fittipaldo VA, Farcomeni A, Scaglione F and Pastori D (2021) A Systematic Review and a Meta-Analysis Comparing Prophylactic and Therapeutic Low Molecular Weight Heparins for Mortality Reduction in 32,688 COVID-19 Patients. Front. Pharmacol. 12:698008. doi: 10.3389/fphar.2021.698008
Received: 20 April 2021; Accepted: 05 August 2021;
Published: 02 September 2021.
Edited by:
Amanj Kurdi, University of Strathclyde, United KingdomReviewed by:
Alejandro Lazo-Langner, Western University, CanadaTanja Mueller, University of Strathclyde, United Kingdom
Copyright © 2021 Giossi, Menichelli, Pani, Tratta, Romandini, Roncato, Nani, Schenardi, Diani, Fittipaldo, Farcomeni, Scaglione and Pastori. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Arianna Pani, arianna.pani@unimi.it
†These authors have contributed equally to this work and share first authorship
‡These authors share senior authorship
 Riccardo Giossi
Riccardo Giossi Danilo Menichelli
Danilo Menichelli Arianna Pani
Arianna Pani Elena Tratta
Elena Tratta Alessandra Romandini1
Alessandra Romandini1 Erika Diani
Erika Diani Francesco Scaglione
Francesco Scaglione Daniele Pastori
Daniele Pastori